Bladder cancer clinical trials hold promise for improving patient outcomes
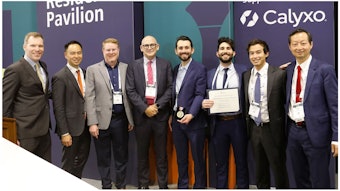
Monday’s Learning Lab showcased leading clinical trials in progress for NMIBC.

Roughly 70% to 80% of patients with non-muscle-invasive bladder cancer (NMIBC) develop recurrence after treatment; roughly 23% of recurrent patients have five or more recurrences. Clinical trials drive new treatments to improve outcomes and quality of life for patients with NMIBC. Monday morning’s Learning Lab featured investigators of 13 clinical trials aimed at developing new organ-sparing treatments for NMIBC, including the three spotlighted in this article.
CUT-less aims to reduce the need for repeat resection Valerio Santarelli, MD,
Valerio Santarelli, MD,
“VI-RADs followed by Photodynamic Transurethral Resection of Non-Muscle-Invasive Bladder Cancer Versus White-Light Conventional and Second Resection: the CUT-less Randomized Trial,” seeks to reduce the risk of a second transurethral resection of bladder tumor (TURBT). The trial will compare the standard of care (re-TURBT) with the preoperative staging accuracy of Vesical Imaging-Reporting and Data System (VI-RADS) and the intraoperative enhanced ability of photodynamic diagnosis (PDD), potentially redefining criteria for re-TURBT indications. “VI-RADs will not replace surgery, but the future is translational and multidisciplinary,” said Valerio Santarelli, MD, the study’s principal investigator from Sapienza Rome University.
MoonRISE-1 investigates a novel drug delivery system
Despite available treatment options for patients with intermediate risk non-muscle-invasive bladder cancer (IR NMIBC), recurrence rates remain high, underscoring the need for novel effective therapies. “MoonRISE-1: Phase 3 Study of TAR-210, an Intravesical Erdafitinib Releasing System, Versus Intravesical Chemotherapy in Patients with FGFR-Altered Intermediate Risk Non-Muscle-Invasive Bladder Cancer,” is investigating TAR-210, a novel intravesical drug-releasing system designed for local delivery directly into the bladder of erdafitinib, a selective pan–fibroblast growth factor receptor (FGFR) tyrosine kinase inhibitor over three months. All visible tumors will be resected at the beginning of the open-label trial. “Recruitment has been robust, with just under 200 sites in 19 countries,” said investigator Roger Li, MD, a genitourinary oncologist with Moffitt Cancer Center.
Urine tumor DNA Study targets cystoscopic surveillance Matthew B. Clements, MD, MS
Matthew B. Clements, MD, MS
Because patients with high-risk (HR) NMIBC have a high recurrence rate, frequent cystoscopic surveillance is recommended. Yet, patients want to be more involved in the decision-making for cystoscopy surveillance frequency—every three to four months for two years—and have fewer of them, if possible. The two-stage-consent randomization trial, “Using Urine Tumor DNA to De-Intensify Surveillance in Non-Muscle-Invasive Bladder Cancer,” aims to identify patients suitable for less frequent surveillance with a urine tumor DNA biomarker test, UroAmp. “Urine Tumor DNA is more sensitive than cystoscopy: 84% versus 53%, to assess response to therapy,” said Matthew B. Clements, MD, MS, assistant professor at the UMass Chan School of Medicine, and the study’s co-investigator. The study will use the UroAmp test to compare the number of cystoscopies in patients with HR NMIBC who received induction of bacillus Calmette-Guérin or gemcitabine/docetaxel and have a negative initial post-induction therapy assessment (negative cytology and cystoscopy ± biopsy), randomizing eligible patients to de-intensified surveillance.