The impact of COVID on sexual medicine
COVID-19 can directly affect testicular tissue and decrease serum testosterone levels.
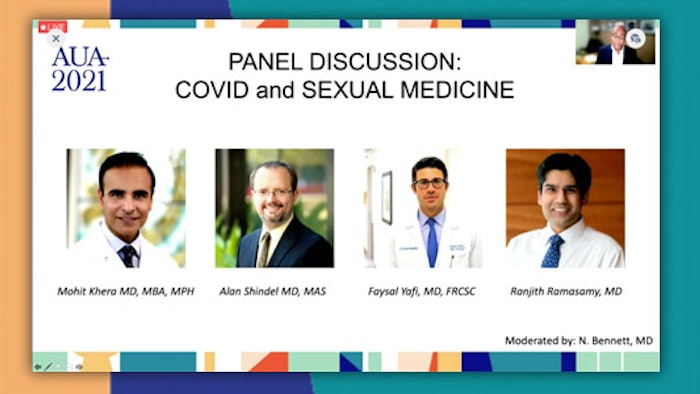
Why does COVID-19 affect men more severely than women? How does COVID-19 affect male fertility? Is there relationship between COVID-19 and testosterone and erectile dysfunction? These are just some of the questions addressed in Sunday’s Plenary panel discussion: “COVID and Sexual Medicine.”
“The potential for COVID-19 to induce significant sexual morbidity is currently overshadowed by the highly morbid and lethal nature of the disease,” said Alan Shindel, MD, associate professor of urology at the University of California San Francisco, whose discussion focused on the endothelial effects of COVID-19 and the potential link to erectile dysfunction.
Down the road, however, COVID-19 may be increasingly relevant as a source of long-term vascular morbidity, including erectile dysfunction.
“Endothelial dysfunction has emerged as a crucial pathway in COVID-19-mediated disease, and endothelial dysfunction is also strongly associated with erectile dysfunction,” Dr. Shindel said. More studies on the chronic nature of COVID-19-mediated endothelial dysfunction are needed.
Why are men at greater risk of dying from COVID-19? “Men have a relative fatality rate from COVID-19 around three-fold that of age-matched women,” said Mohit Khera, MD, MBA, MPH, professor of urology at Baylor College of Medicine in Houston. Could male testosterone be the culprit? It depends.
“Normal levels of testosterone may increase viral entry while paradoxically providing a relative protection from the hyperreactive immune state that drives COVID-19 mortality,” Dr. Khera said. Still, COVID-19 can directly affect testicular tissue and decrease serum testosterone levels.
“Low serum testosterone levels have been associated with worse clinical outcomes and increased mortality in those infected with COVID-19, butt it is still not fully understood whether testosterone therapy impairs or improves COVID-19 outcomes,” Dr. Khera said.
COVID-19 has pushed telemedicine to become mainstream; telemedicine was used by 70% of urologists in 2020 compared with just 14% previously, said Faysal Yafi, MD, assistant professor of urology, chief of Men’s Health and Reconstructive Urology and director of Men’s Health and Newport Urology at the University of California, Irvine.
Sexual medicine is a burgeoning telemedicine area. Although online direct-to-consumer sexual medicine companies such as Hims and Roman, which seek to give customers treatment services for erectile dysfunction and other men’s health issues without relying on traditional healthcare systems, continue to expand, “there are reimbursement and HIPAA uncertainties. Licensure requirements may be problematic,” Dr. Yafi said.
Another drawback: Direct-to-consumer sexual medicine is expensive. Dr. Yafi noted that the cost of telemedicine visits for sexual health issues with a conventional physician can cost patients less.
Could COVID-19 impact male fertility? Ranjith Ramasamy, MD, director of reproductive urology and an associate professor in department of urology at the University of Miami in Florida, established that COVID-19 is able to evade the immune system and exist in organs long after the initial infection.
“SARS-CoV-2 is present in both testis and penile tissue but not in semen,” Dr. Ramasamy said.
Still, COVID-19 won’t likely result in chronically reduced sperm counts.
“COVID-19 infection appears to impact sperm parameters in three to six months, but sperm appear to recover after that period,” Dr. Ramasamy said. Moreover, the COVID-19 vaccine does not appear to impact male fertility, he said.
Visit AUA2021 Daily News Online for more articles.