Neurogenic bladder treatment evolving
Is the proactive approach best, or is reactive management better for young patients?
Children with neurogenic bladder have traditionally been managed reactively, with management driven by demonstrable clinical changes. A more proactive approach has emerged in recent years, driven by early and regular assessment of renal and bladder anatomy and function, imaging and laboratory testing. The latest results from the ongoing Urologic Management to Preserve Initial Renal Function in Infants and Young Children with Spina Bifida (UMPIRE) study could help shape the course of future treatment.
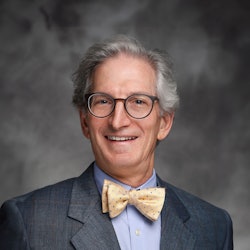
“Reactive management is less invasive and less costly,” said John Wiener, MD, professor of urology and of pediatrics at Duke University School of Medicine in Durham, North Carolina. “The proactive approach has a low threshold to initiate clean intermittent catheterization and medical therapy to optimize bladder emptying, minimize bladder storage pressures and protect the kidneys.”
The superiority of the proactive approach has not been proven in terms of long-term renal outcomes, Dr. Wiener said, but more proactive management has been increasingly adopted to reduce morbidity. The continuing analysis of UMPIRE, a 10-center study launched in 2015 through the Centers for Disease Control and Prevention, may inform the debate.
UMPIRE focuses on children with neurogenic lower urinary tract dysfunction who have the myelomeningocele form of spina bifida from birth to 10 years. Spina bifida is the most common, but not the only, cause of pediatric NLUTD. Dr. Wiener was one of the earliest study investigators.
Dr. Wiener will chair a panel discussion of the latest findings from UMPIRE in “Management of Neurogenic Bladder—Update on Current Options” during the Plenary on Sunday from 8-8:20 a.m. in the Stars at Night Ballroom. He will be joined by Evalynn Vasquez, MD, associate professor of clinical urology at Keck School of Medicine of the University of Southern California; M. Chad Wallis, MD, professor of surgery and chief of pediatric urology at the University of Utah in Salt Lake City; and Douglass Clayton, MD, associate professor of pediatric urology and medical director of the Multidisciplinary Spina Bifida Clinic at Vanderbilt University Medical Center in Nashville.
NLUTD is one of the most vexing challenges in pediatric urology, Dr. Wiener noted. Management is changing, but the goals of care continue to focus on preservation of renal function, minimization of urinary tract infections and progression toward urinary continence. Many children and caregivers also work on improving empowerment to gain independent bladder management and avoiding significant disease-related and treatment-related complications.
“Few disorders in pediatric urology receive more attention than NLUTD,” he said. "Despite its relative rarity, inadequate treatment can lead to decreased quality of life, renal failure and even death. Fortunately, a combination of collaborative research efforts, newer pharmacologic agents and efforts to reduce short-term and long-term surgical morbidity portend a brighter future for affected children, their caregivers and the health care community.”