What is the future of telemedicine in sexual medicine?
Sunday’s plenary promises to offer a healthy debate about the benefits and disadvantages of telemedicine.
COVID-19 helped propel telemedicine into the mainstream, allowing patients to continue receiving health care but from the convenience of their homes. What’s next for the post-pandemic era? How will telemedicine shape the future for patients and providers in sexual medicine?
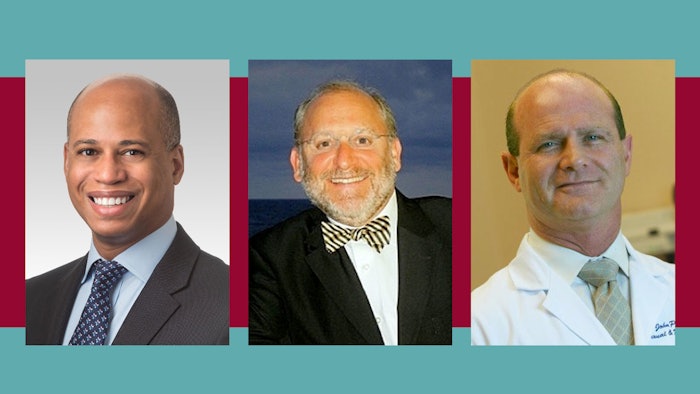
“There are many pros and cons to telemedicine that weren’t discovered until we entered into the pandemic and started using it more frequently. It’s a constantly evolving landscape,” said Nelson E. Bennett, MD, associate professor of urology and director of sexual medicine at Northwestern University Feinberg School of Medicine in Chicago. Dr. Bennett will moderate Sunday’s plenary, “Crossfire: Clinical Controversies in Urology Debate: Telemedicine Is Good for Patients and Providers in Sexual Medicine.”
Should telemedicine in sexual medicine continue in the post-pandemic era? In Sunday’s debate, John P. Mulhall, MD, MSc, FECSM, FACS, FRCSI, director of Male Sexual & Reproductive Medicine at Memorial Sloan Kettering Cancer Center in New York City, will build the case that continuing telemedicine in sexual medicine is good for providers and patients, especially those patients who don’t live close to a medical facility. It also could be an essential tool for reaching underserved populations and potentially used to offset workforce shortages. Dr. Mulhall will discuss the benefits of telemedicine in sexual medicine and best practices for implementing the technology seamlessly into your practice and workflow.
Gerald B. Brock, MD, FRCSC, professor emeritus in the Department of Surgery, Division of Urology, at Western University in London, Ontario, Canada, will present the counter argument: Telemedicine is a detriment for patients and providers in sexual medicine and that the use of telemedicine technology may put some providers and patients at a disadvantage, including patients who don’t have a traditional computer, lack high-speed internet access in their homes or who have a limited cellular data plan. Dr. Brock will also outline other limitations of telemedicine in sexual medicine, including how effectively it delivers patient care, especially with the lack of a physical examination.
“Generally, anytime you need to examine a patient, whether for diagnostic purposes or for postsurgical follow-up, you need to see them in person,” Dr. Bennett said. “With new sexual medicine patients, it’s important to look at their body language and facial expressions and hear the inflections of their voice. It’s challenging to pick those up on a video or telephone conversation. But telemedicine can be convenient for follow-up patients on maintenance therapy.”
Still, do the advantages of sexual medicine telemedicine outweigh the downsides? Sunday’s session will highlight the pros and cons to help you decide whether to continue to integrate telemedicine into your practice or to consider phasing it out in the future.